Is Lowering Cholesterol The Top Priority For Resolving Stroke Or Heart Attack Risk?

In mainstream medicine, there is a fixation on cholesterol levels as a determinant for whether or not you have a condition that could put you at risk for heart/cardiovascular event (like a heart attack or stroke) .
Is it true that watching your cholesterol levels to make sure they stay in a so called “safe range”, the saving grace for preventing an event, like a stroke or heart attack? Or are there other far more crucial causal factors to take account for?
In this piece we will examine what cholesterol is, the biological function of LDL (bad cholesterol) and HDL (good cholesterol) and why the medical and pharmaceutical industry at large, proclaim that cholesterol is the main culprit for declining health issues like heart disease and angina.
Then we will look into other potential causalities that could be identified and addressed, outside of the paradigm and purview of allopathic medicine, other than just the conventional approach which involves lowering your cholesterol to specified (safe) levels through modalities such as, prescribed statin drugs and a cholesterol free diet.
So, lets see if we can untie some knots, so as to better understand how and why cholesterol has been much maligned for over half a century and pose the question: should it be?
What Is Cholesterol And It’s Function?
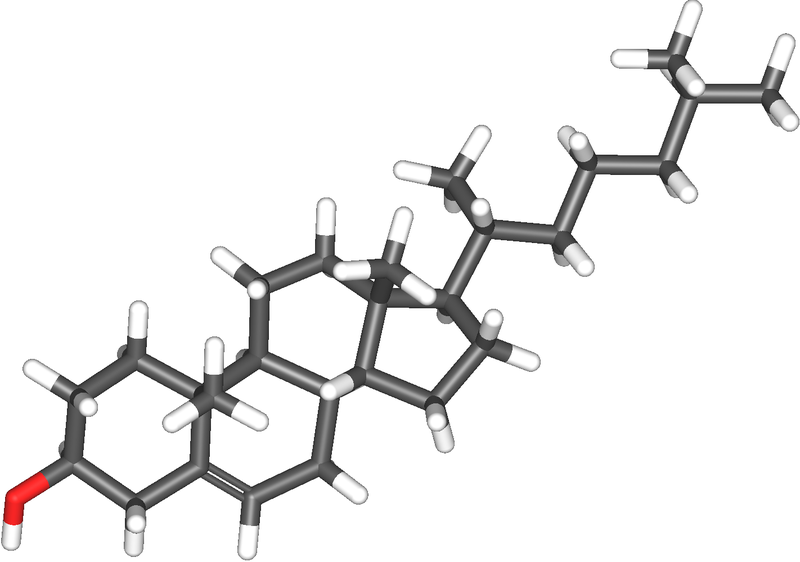
Cholesterol is a significant element of the sterol class that aids in healing. As a chemical compound that the body requires, it is a building block for cell membranes and for hormones like estrogen and testosterone. It is often referred to as a waxy substance in the blood.
Biologically speaking, cholesterol is considered to be one the most intricate molecules in the world. It has been shown to be essential in more complex living beings.
It repairs arterial inflammation by combining with other substances that form “plaque” to heal the arterial lining. It provides for the formation of cell membranes and structurally fortifies them to protect cell walls , as well as, producing hormones and vitamin D.
Another key role for cholesterol is to act in synthesizing bile acids.
There are numerous other processes that take place in the body which are vital to sustaining health. Many of these processes require cholesterol.
Cholesterol’s vital benefactors
Why is cholesterol important to bodily function and structure?
- The brain, nerves, muscle, skin, liver, intestines and heart are manufactured from it
- Steroidal sex hormones (estrogen & progesterone in women and testosterone in men) and adrenal hormones (cortisol and aldosterone) are produced from cholesterol
- Regulates temperature and fluidity of the cell membrane
- As touched on above, cholesterol plays a role in the creation of bile salts. Like cholesterol, bile salts are produced in the liver, then stored in the gallbladder. They aid in digestion/assimilation and uptake of fat and vitamins A,D,E and K.
- Regulates synthasis of Vitamin D, which amoung other things, is responsible for the absorption of calcium
- It is mostly concentrated in the brain
Cholesterol production is carried out by a sequence of responses. This is a complicated fusion that involves 37 actions. This process starts in the liver with an essential enzyme referred to as HMG-Coa reductase by way of the mevalonate pathway.
In order to manage the amount of cholesterol in the body, a response action takes place in which cholesterol synthesis is slowed down in the liver. This occurs when the dietary intake thereof, rises. Conversely, the same process takes place when dietary cholesterol intake drops, which prompts elevated synthesis in the liver.
When too much cholesterol is present in the body, it can build up in deposits or plaques along the inside walls of arteries, causing them to narrow.
Where Is Cholesterol Derived From?
Cholesterol is acquired in the body from two different class sources: serum cholesterol and dietary cholesterol.
The liver produces about 80% of the body’s (serum) cholesterol and the rest comes from dietary sources like meat, poultry, eggs, fish, and dairy products. Foods derived from plants contain no cholesterol.
Cholesterol content in the bloodstream is regulated by the liver. After a meal, cholesterol in the diet is absorbed from the small intestine then metabolized and stored in the liver. As the body requires cholesterol, it may be secreted by the liver.
So, in a nutshell our bodies are predominately capable of producing and regulating proper cholesterol levels when health is in proper balance.
Understanding Lipoproteins and triglycerides
Cholesterol has a very close relationship with lipoproteins and triglycerides.
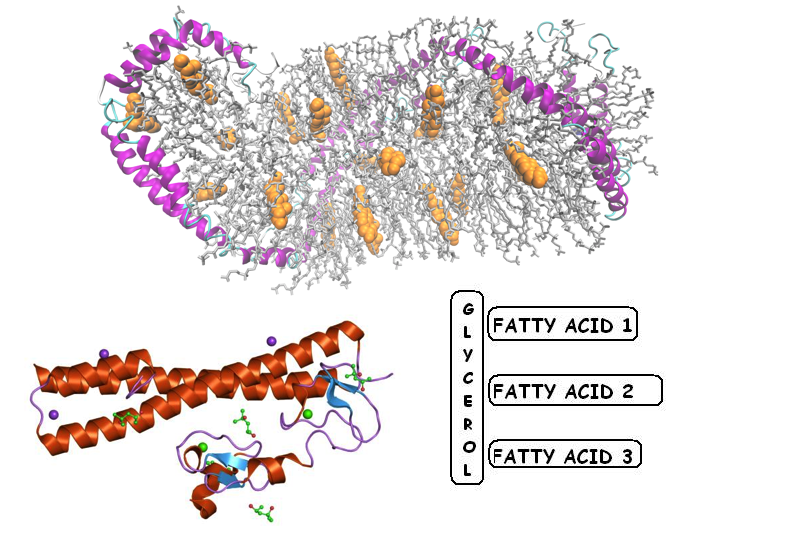
Lipoproteins are biochemical packets produced from lipids and proteins. They are instrumental in moving fats across cellular membranes as well as the circulatory structure. This is done by binding to fats and assimilating them.
Since cholesterol does not travel freely through the bloodstream on it’s own, it needs some help. It is attached or carried by lipoproteins (lipo = fat) in the blood. There are four types of lipoproteins that are categorized based upon how much protein there is in relation to the amount of cholesterol. Density is another marker for classifying lipoproteins.
The larger lipoproteins are not as dense as smaller lipoproteins and consist of more fats than proteins.
Lipoprotein types
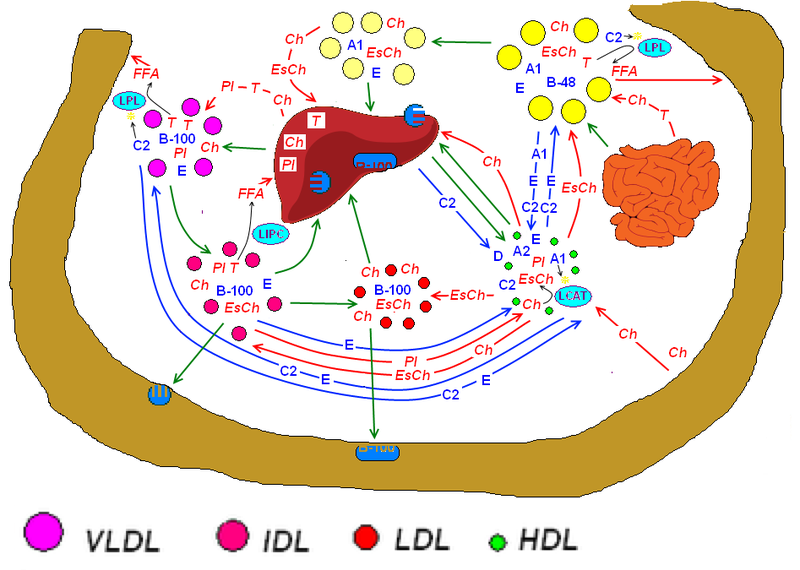
Low-density lipoproteins (LDL) contain a higher ratio of cholesterol to protein and are thought of as the “bad” cholesterol. Elevated levels of LDL lipoprotein are considered a risk for heart disease, stroke, and peripheral artery disease, due to the buildup of cholesterol plaque along the inside of artery walls.
Over time, as plaque buildup (plaque deposits) increases, the artery narrows (atherosclerosis) and blood flow decreases. If the plaque ruptures, it can cause a blood clot to form, which constricts blood flow. This clot is the cause of a heart attack or myocardial infarction if the clot occurs in one of the coronary arteries in the heart.
The liver is responsible for managing the levels of LDL and bringing it where it is needed in the body. It manufactures and secretes LDL into the bloodstream. There are receptors on liver cells that can “monitor” and “adjust” the LDL levels. However, if there are fewer liver cells or if they do not function effectively, the LDL level may rise.
Research has shown evidence that the smaller more dense LDL molecules are a better indicator than total LDL for determining atherosclerotic plague levels that could put you at risk and (or) cause cardiovascular and heart disease (more on this later).
A standard recommendation is for total LDL levels to be below 100 mg/dl according to ATP Ⅲ guidelines.
Here is a type of subclass identification that breaks down LDLs into 2 different catagories:
- Pattern A are the larger more fluffy LDLs which are considered a non factor in the development of atherosclerosis. Essentially, these are harmless.
- Pattern B denotes the smaller more dense molecules. These are the ones that can pose a danger to heart/cardio vascular health as there is a 3 to 5 fold escalation for heart attack risk.
High-density lipoproteins (HDL) are made up of a higher level of protein and a lower level of cholesterol. These tend to be thought of as “good” cholesterol. It is commonly claimed that the higher the HDL to LDL ratio, the better it is for the individual because such ratios can potentially be protective against heart disease, stroke, and peripheral artery disease.
One reason HDL is considered “good” cholesterol is due to it’s task in removing excess cholesterol from the bloodstream to the liver. It has been described as a wheelbarrow to transport LDL off of the arterial walls. From there, it is broken down and eradicated before the build up of arterial plague can occur in the arteries.
Very low-density lipoproteins (VLDL) are manufactured in the liver from triglycerides, cholesterol and apolipoprotein B. VLDL breaks down into Intermediate density lipoprotein (IDL) once it goes into the blood stream. Thereafter, the adipose tissues and muscles uptake fatty acids after they are broken down. They contain even less protein than LDL. In addition, they deliver triglycerides from the liver to adipose tissues. VLDL like LDL has been associated with plaque deposits.
Intermediate density lipoprotein (IDL) is scarcely detected in the blood. This particular lipoprotein is produced as an intermediary step in the regular metabolism of VLDL. It is either brought back to the liver or transformed into LDL. The LDL manufactured from this process has a high cholesterol content.
There is a subclass of lipoprotein referred to as lipoprotein (a). This class of lipoprotein is said to be one of the best markers for determining whether one is at risk for heart attack or stroke.
What are triglycerides

Total cholesterol score is the sum of HDL cholesterol, LDL cholesterol and 20% of triglycerides as determined by a blood test. A high score suggests an increased risk for developing cardiovascular disease and/or strokes.
Some factors that are known to be responsible for high triglyceride levels:
- Excessive weight or obesity
- sedentary lifestyle
- cigarettes
- alcohol (in excess)
- high carb diet
The standard recommendation for an optimum triglyceride level is 150 mg/dl.
Cholesterol: Ally or Adversary?
For over 50 years cholesterol has been targeted in a negative light as a present risk to cardiovascular/heart health even though it is a structural element in all cells..
Conventional medicine lends itself to the paradigm that higher cholesterol levels lead to diminishing cardiovascular health that puts you at higher risk for heart attack or stroke.
It also has been vilified as the reason for a type of degeneration that manifests in the narrowing and hardening of the arteries, known as atherosclerosis.
There are scenarios in which cholesterol levels can be out of balance, which can result in a condition known as hypercholesterolemia. While in this state, high levels of LDL are produced along with low levels of HDL. There is much data out there implying that this is a significant threat for heart attack, stroke and peripheral vascular disease.
More than cholesterol itself, it is the high levels of LDL that are said to be the true threat and the notion of just merely lowering cholesterol levels alone is not going to mitigate the risk of heart disease.
Diet and genetics both play a factor in a person’s cholesterol levels. There may be a genetic predisposition for familial hypercholesterolemia (hyper=more = cholesterol + emia=blood) where the number of liver receptor cells is low and LDL levels rise causing the potential for atherosclerotic heart disease at a younger age.
In the diet, cholesterol comes from saturated fats that are found in meats, eggs, and dairy products. Excess intake can cause LDL levels in the blood to rise. Some vegetable oils made from coconut, palm, and cocoa are also high in saturated fats.
Since the body stores cholesterol in the liver to be reused, the body regards cholesterol to be significant in operating efficiently.
Strange as it seems, an individual’s cholesterol can be very high and and still have pristine clean vessels. While at the same time, someone could have low cholesterol and be afflicted with corona.
Dr. Arthur Agatson, a cardiologist and best selling author/creator of the The South Beach Diet, states that in his practice he has seen diabetics with cholesterol in the normal range that are afflicted with coronary disease and those who have high cholesterol and have immaculately clean arteries.
He goes on point out that an individual should be not be reassured by specific levels of cholesterol, particularly if there is a genetic history of heart disease and other cardiac risks.
Additionally, there are studies like this one that demonstrate statistics to show that at least half of those who fall victim to a heart attack have total cholesterol levels within a normal range.
Cholesterol: the good and the bad
Dr. Berg explains the truth about cholesterol
More insights into the benefits and vilification of cholesterol
In this radio broadcast from 2017, Dr. Jenifer Daniels offers a comprehensive interpretation of the essential health benefactors of cholesterol and why it has been misunderstood as a malignant scourge against heart and cardiovascular health. Listen here
Is cholesterol the culprit behind atherosclerosis?
Looking at the tenancies in modern medical science, there is a bent on citing cholesterol as an instigator in the development of atherosclerotic plaque.
These facts are only withstanding if their is a relationship between cholesterol levels and atherosclerotic plaque build-up.
In 1961 Dr. K. S. Mathur M.D. and his colleagues performed studies to verify a correlation between total cholesterol and atherosclerosis.
The barometer used to undertake this study involved measuring the level of total cholesterol and the corresponding magnitude of atherosclerosis in 20 deceased patients and 200 more cases obtained from medical libraries. Subjects were tested within 16 hours of death.
The conclusion divulged that there was no tie-in between blood cholesterol levels and atherosclerotic plaque.
In a 1962 issue of The American Heart Journal, research from another postmortem study was published showing that, out of 106 cases studied, it was confirmed that of those who suffered from atherosclerosis had a 35 mg. per cent higher average level of cholesterol in their blood than those who did not have atherosclerotic damage.
Though the statistics show evidence that a higher level of cholesterol was present in atherosclerosis cases, the margin is considered slim enough to construed as insignificant in the overall group. However, of the cases that showed advanced atherosclerosis and sudden death from coronary sclerosis in the group, a significantly higher level of cholesterol was found.
Then again, the average serum cholesterol level was lower in the sub group who died from cardiac infarction as compared to the group who had suffered from sudden coronary death.
There have been many autopsy studies dating back to 1936. A common thread that runs though these studies is, that many published findings show cholesterol levels not to be correlative with the sum of atherosclerosis found in those examined. Read more here
More on this later in the piece
Is high HDL always good?
According to a study started in 1987 and completed in 2011, it was determined that high HDL is not always helpful. The study makes for some very compelling results lending to the prognosis that when HDL levels are increased, then so are the amount of LDL and triglycerides in the blood.
So the study’s takeaways strongly suggest that simply raising HDL in and of itself may not contribute anything to overall health and could very well be harmful to heart and cardiovascular health. It also may be worthy of taking into consideration that when taking drugs and or consuming a cholesterol rich diet, that this could be a cause for HDL buildup in the blood.
When this occurs, it is hypothesized that when HDL stays in the blood longer than it should, that there is a strong possibility that it will be oxidized (as compared to a metal pipe building up rust) resulting in unwanted health consequences.
Another study from a National Institute Of Health (NIH) clinical trial, performed in 2011, recruited a group of participants who took an FDA approved niacin product called “Niaspan” with the purpose of raising their HDL and lowering LDL and triglycerides.
During the 32 months of the 6 year trial (which was discontinued) the results demonstrated that there was no reduction in fatal or non-fatal heart attacks, strokes or hospitalizations. This is regardless of the fact that those participants had raised HDL and reduced LDL and triglyceride levels.
In comparison, the other group (whom was given a statin alone) did show a reduction in such events.
As is fairly pervasive with FDA approved drugs and other treatments, “Niaspan” has been associated with some very precarious side effects including:
- Toxicity and inflammation to the liver
- Ulcers
- Headaches
- Elevated risk for gout
Question: Could it be that such a treatment that causes these side effects, and especially, compromises the health of the liver in this way, be cause for a condition that is toxifying the bloodstream in some way that leads to the results in the study?
Furthermore, does it bring question to the merits of the study if the premise is to ascertain what raising HDL along with lowered LDL and triglycerides does to reduce the risk of heart attack or stroke? Would this be the case if the study was conducted using diet, exercise and supplementation instead of a pharmaceutic approved drug like Niaspan?
More on HDL as it refers to “testing” further in this piece.
Is high (total) LDL the problem?
As mentioned earlier, LDL exists in different sizes/density in the body and in particular, the bloodstream. Could it be that the commonly purported idea that LDL as a whole, being responsible for elevated risk for heart attack or stroke, is flawed?
Maybe we should be looking at the different sub-classes of LDL. The smaller LDL particles are much denser that the larger LDLs and thus have been shown to wedge themselves into the artery walls, leading to atherosclerosis. On the other hand, large LDL molecules are to large to get in to the creases of those walls.
Still, most medical doctors are trained and fixated on pushing the narrative of lowering total cholesterol.
The National Cholesterol Education Program in 2004, recruited a panel of 9 doctors to contribute recommendations for the reduction in the risk of heart disease. The panel presented the conclusion that LDL should be kept at a maximum of 100 mg/dl.
However, in a review from the Annals of Public Medicine in 2006, the authors seeked out to obtain data from all controlled, cohort and case controlled studies to examine an independent relationship between LDL levels and cardiovascular repercussions to verify cause for the panel’s recommendations.
The study failed to produce any substantial evidence to support those recommendations (including the panal’s own published studies).
In addition to the authors’ findings, it was also purported that 8 out of the 9 paneled doctors received financial contributions from drug companies who sell these cholesterol lowering drugs (like statins).
Despite all this, The American Heart Association still follows the guidelines based on the recommendations of the NCEP doctor’s panel. Read the full report here
What are the risks of lowering cholesterol?
Since cholesterol plays a vital role in many biological processes, what are the specific health consequences of significantly lowering cholesterol? Is the risk worth the upside?
Here are some factors to take into account:
Reduction in the production of vitamin D
A notable source of vitamin D synthases occurs through the skin via ultraviolet sunlight by irradiating a cholesterol metabolite. This simulated pathway is critical in keeping vitamin D levels up and promoting synthesis. Low cholesterol levels can severely compromise this activity.
Other key molecules
Cholesterol also functions as a precursor in synthesizing other necessary molecules. Of these, are all steroidal hormones which are contingent on ideal cholesterol level in the blood.
When cholesterol levels become extremely low the endocrine and reproductive system can be badly compromised.
Low fat diet and the risk of disease
In countries like the US and Australia, meat and diary consumption has remained steady for the last 4 decades or so. However, in that span there been less consumption saturated fat and cholesterol, while the consumption of low fat, highly processed and highly marketed items produced by the major food industry, is on the rise.
Due to the content of transfats, refined carbohydrates and high fructose in these foods, the dietary habits in these parts of the world would seem to explain the weight/obesity/diabetes epidemic and how it could very well be systemically related to the increase in heart disease over these decades.
Scientists at the University Of Harvard performed a study back in 2013 which showed many streams of evidence that it is not the amount of fat intake, in and of itself, that manifests the danger in coronary heart disease (CHD) but rather the types of fats we consume.
In fact, the study yielded an results from the epidemiological studies and controlled clinical trials that showed that saturated fat, as opposed to unsaturated fat, is far more valuable in reducing CHD risk than total fat consumption.
Further more, this reveals that the idea of a low fat diet as a means to lose weight, holds no weight, so to speak. Additionally, replacing these fats with carbohydrates is far more likely to cause one to gain weight.
So, this offers strong credence to the notion that the total sum of saturated fat in the diet likely has little, if any, impact on heart disease risk.
More details of this are covered in the book and documentery
: “In Defense Of Food: An Eaters Manifesto” by Michael Pollan.
sources: 1,3,8,12,15,17,18,19,21,23,25,26
Safety Considerations For The Use Of Cholesterol Lowering Drugs
Tops on the list for most prescribed medications in the US are Antidepressants, painkillers and Cholesterol Lowering Drugs. There are several health and wellness pundits who decry these drugs as useless and proclaim that they could cause undesirable side effects/health risks.
Statins:
The most popular sub-class of prescribed cholesterol lowering drugs are statins. These drugs have been associated with numerous side effects such as:
- weakness and pain in muscles
- acidosis
- anemia
- cataracts
- sexual impotence
- diminishing memory and cognitive functions
- liver and pancreatic impairment
- decreased immune function
- elevated risk of cancer
Statins function by way of restricting an enzyme mentioned earlier: HMG-Coa reductase. Besides this enzyme, which is active early on in the process of cholesterol synthesis, the same pathway is also important in facilitating the production of other functional compounds and sterols such as dolichols.
The sterol dolichol is an important component in the communication, identification and maintenance of cells. The suppression of dolichols via statins has been associated with neurological disorders such as transient global amnesia.
In addition, the production of coenzyme Q10 (which is vital for muscle strength), sex hormones, adrenal hormones and vitamin D is inhibited by statins.
Do cholesterol lowering drugs really work?
A little over a decade ago Merck conducted a clinical trial of the cholesterol drug Vytorin. The conclusion of this trial was delayed for about 2 years, while in the mean time, the FDA granted approval for the drug. When the trial was finally concluded, the data revealed that the drug showed no reduction in the build up of arterial plaque.
In another clinical study, Lipitor presented misleading results claiming that it could reduce heart attack risk by 36%. However, the study actually showed that 3% of the placebo group had heart attacks or death as compared to 1.9% of the Lipitor group.
links from sourced references: 1,16,19,20,24,27,28
Assessing Solutions For Managing Cholesterol And Cardiovascular/Heart Risk
In mainstream medicine, your doctor will likely tell you that you need to lower LDL and Raise HDL if your cholesterol is considered high. In accordance with AHA guidelines, it is recommended that following a dietary regimen that includes fruits, whole grains, legumes, poultry, omega 3 rich fish and unsaturated fats such as olive oils, avacodo oils and nuts.
Inversely, the AHA’s guidelines highly recommend limiting the consumption of sugar sweetened foods and beverages (sports drinks sodas and juices).
The guidelines also stress the importance in limiting saturated fats and trans fats to 5% of total daily calories.
In addition, the AHA’s guidelines also advocate for making time to incorporate moderate intensity physical activities at a baseline of 3 or 4 times a week for around 40 minutes.
Established science has been steadfast in maintaining that there is a strong connection between cholesterol and the plausibility of heart disease. Although this a considered a common truism, what hasn’t been settled is the smoking gun evidence that cholesterol is the cause and not merely a bystander at the scene.
One of cholesterol’s major functions in the body is to repair damage from inflammation to arterial walls. So, given the fact that cholesterol in the blood increases as a healing response, it would make sense that there would be a correlation with damaged/inflamed arteries.
So we come to the question: wouldn’t that make inflammation, that leads to subsequent arterial plaques that build up in the process of healing (after the fact), the perpetrator behind this cycle?
More on inflammation further in this piece
Another caveat to take into consideration is that, the body in a healthy state should be able to pass an excess of cholesterol but this could be problematic if you have digestive problems (which is covered further in this piece and is another growing epidemic as is written about in one of my earlier posts).
Testing For Cholesterol And Other Heart/Cardiovascular Risks:
The American Heart Association recommends that all adults beyond the threshold of 20 or older should have their cholesterol (as well as other possible threats to cardiovascular/heart health) checked at least every six years.
A typical test will show blood cholesterol levels as measured in milligrams per deciliter (mg/dl). The doctor uses this metric to anticipate whether or not you have long or short term risk for heart attack or stroke. Other variables that are factored in are: age, genealogy (family), smoking and high blood pressure.
Another type of test, referred to as a complete cholesterol test or a lipid panel/lipid profile will normally provide results for HDL, LDL, VLDL, triglycerides and total blood (serum) cholesterol.
Testing HDL
In recent years, doctors have been using more extensive methods for evaluating HDL by way of factoring in other risk aspects. One of the results of this test has indicated that a high triglyceride reading is linked with lower HDL, which the evidence suggests causalities such as, genetics, type 2 diabetes, weight problems, and sedentary lifestyle are determinants.
Now, there is another angle (covered later in this article) that suggests the testing results that show your total cholesterol to HDL ratio, is what you should be paying close attention to.
Testing LDL
Like HDL, LDL testing today involves many other aspects besides just probing LDL levels. This also, is in accordance with American Heart Association guidelines. It is suggested that you discuss testing LDL with your doctor.
This facet of testing involves an amalgamation of various measurements. As mentioned above, this is done by figuring in your total cholesterol score, which entails adding HDL and LDL levels with 20% triglyceride levels.
As alluded to above, the complete cholesterol test will look at all aforementioned lipoproteins. However, this test does not differentiate between the “safe” pattern A LDLs and the “unsafe” pattern B ones. So how can you know whether you have dangerous pattern B LDL levels?
Evaluating your triglyceride levels in conjunction with your total LDLs may be the answer. In other words, if your LDLs and triglycerides are high then you will have a higher concentration of pattern B LDLs. Whereas, if your triglycerides are low and your LDLs are high you will have a higher concentration of the benign pattern A LDLs.
Ayurvedic recommendations, in terms of testing, include a fasting test wherein where you fast for at least 12 hours before a blood draw in order to yield more accurate results. After the results have been processed, you will make a determination based on your triglyceride to LDL ratio (not the individual scores).
If your LDLs are high and your triglycerides are low then you should be fine but, if both are high then it important to account for that and make the proper adjustments such as: reducing stress, eliminating processed sugars and improving digestion.
What are considered healthy cholesterol scores?
The The American Heart Association’s NCEP risk guidelines advocate following these numbers:
| Total Cholesterol (mg/dL) | |
|---|---|
| < 200 | Desirable |
| 200 to 239 | Borderline high |
| > 240 | High |
| HDL (mg/dL) | |
| < 40 | Low |
| > 60 | High |
| LDL (mg/dL) | |
| < 100 | Optimal |
| 100 to 129 | Near Optimal |
| 130 to 159 | Borderline high |
| 160 to 189 | Near high |
| > 190 | High |
What numbers should you be aware of when you assess your HDL levels?
Earlier in this piece we covered the suggested risks of total cholesterol being in a range (200 mg/dl or over) that is commonly construed as threatening.
Many, including this Functional medicine expert, among others, recommend focusing more on the ratio of cholesterol/HDL than total cholesterol. A suggested optimal ratio is 3.0.
For example: If you’re total cholesterol was 240 mg/dl (200 or under is commonly considered safe) and you’re HDL is 80, your cholesterol/HDL ratio would be 3.0 (240%80). Whereas, if your total cholesterol was 180 (which is commonly considered desirable) and your HDL was 25, your ratio would be 7.2 and would pose a higher heart health risk due to the low HDL.
It has been stated that there are many with a total cholesterol score of 300 but a very high HDL to aid in maintaining the recommended ratio, and do not have coronary plaque.
Other types of testing that don’t include cholesterol
CRP (c-reactive protein) test – This is a test that measures inflammation in the body. The accuracy of the test is still developing so, it still needs work. Nevertheless, this method of testing appears to be a far better indicator for evaluating heart risk that a total cholesterol test.
More on confronting the causes of inflammation further in the next sub section.
Homocysteine test – Homocysteine is an amino acid that is found in the bloodstream and has been connected with heart disease and stroke. This test focuses on measuring your serum homocysteine levels.
Getting the above tests:
The first choice is to ask your doctor about having the tests done.
If the above is not possible, there are online services that offer a fairly inexpensive CRP test and homocysteine test that you can purchase and get tested in your area. No doctor or insurance required.
Particle size test – The premise of this test is to determine the amount of “B particle” LDLs, which are the small denser ones that get lodged in the walls of the arteries and can promote inflammation that can lead to blockages.
Electron beam computed tomography (EBCT) – EBCT is a cutting edge imaging technology that that takes x-rays of the heart and coronary arteries. It differs from a ct scan in that, instead of taking images that show portions of your heart, the EBCT camera mechanism moves in spiral. This makes for clearer images of the heart even though the camera is moving.
This method is particularly effective in obtaining a calcium score, which is another marker for determining your risk for cardiovascular/heart disease and (or) atherosclerosis. Although not as precision as an EBCT scan, a calcium score can also be acquired with a ct scan.
The downside of this test (as it is with other such tests like ct scans) is the radiation exposure which is something to enter into the equation for consideration.
Dietary considerations for managing cholesterol and heart health
Managing LDLs
Lets look further into pattern A and pattern B LDL types.
Pattern A has been identified as the safe LDL. Dietary (healthy) fats only raise this subclass of LDL .
Here are some foods that are in rich in fats:
Flaxseed, Almonds, Olive oil, Virgin coconut oil, Fish (omega 3s), Peanuts, Clarified butter, Ripe olives, Peanut oil,, Hemp seed oil, Pecans, Cashews, Dark chocolate
Pattern B, the unhealthy subclass, is produced from fructose.
Foods high in fructose:
Soda, Candy, Sweetened yogurt, Salad dressing, Canned fruit, Cereals, Artificially sweetened Juices, Coffee creamer, Jams and jellies, Sports drinks, Ice cream, Condiments
Digestion
In Ayurvedic medicine there is a term referred to as “Agni” which means digestive fire. When consuming too many hard to digest foods this “digestive fire” can go out of balance. When Agni is diminished, the body is not able to digest and pass an overabundance of cholesterol.
Here are some suggested food items to be avoided that can deplete digestive agni:
- Excessive sweets
- Dry foods
- Processed foods
- Cow milk and genetically modified wheat – Which can be responsible for constipation and a sickly intestinal microbiome that could lead to leaky gut syndrome. This can trigger an inflammatory response in the bloodstream.
Foods that can promote digestive agni:
Ghee. This is a a form of clarified butter that is altered by removing milk solids and other impurities. Leftover, is the healthy fats. It is a cooking oil that has been used for thousands of years and promotes healthy digestion and metabolism (agni) among other incredible benefits.
Ghee is very easy to make as you can see here. Or you can get it here.
For more on digestion, see my post: Firing Up The Furnace.
Here are some nutrients/supplements that can be helpful in raising HDL:
- Niacin
- Acetyl-L-Carnitine
- Taurine
- Magnesium
- Phosphatidyl Choline
- Vitamin E/Tocotrienols
More suggested items to add and subtract from your daily consumption
- Stop smoking: smoking can weaken arterial walls and make you deficient in HDLs.
- Pistachio nuts and mushrooms: have these in your diet as they can mitigate symptoms of metabolic syndrome or heart/ cardiovascular disease.
Other avoidances to be aware of that can diminish heart health
- Inadequate dental hygiene – An 8 year study published in the British Medical Journal (2010) found that insufficient oral hygiene has an association with cardiovascular disease and inflammation.
- Xenoestrogens – These are molecules that are foreign to the body and are found in plastics, soaps/detergents and personal care products. This could cause an inflammatory result in your arteries.
- Electromagnetic Frequencies (EMFs) – The radiation from these frequencies have been known to provoke arterial plague due to the oxidizing of LDLs. Since these frequencies are emitted from cell phones, cell towers, wifi towers, microwaves, hairdryers, televisions ect…., we can’t completely eradicate them from our lives. We can though, mitigate exposure in our homes by taking measures such as, eliminating hair dryers, microwaves and keeping your cell phone and other EMF emitting devices/electronics away from your bedroom (15 feet or more) when turning in for the night (for starters).
- Heavy metals – Exposure to heavy metals (like mercury) can be harmful to the heart muscle. ETDA (a chelation therapy) has shown positive results in chelating arterial plaque buildup. Although it should be noted that, it has also been linked to certain side effects.
- Insecticides and pesticides – Subjection to these chemicals can set off autoimmunity leading to inflammation. When purchasing fruits and vegetables make sure they are organic and (or) make sure you rinse them well before eating.
- Inadequate Sleep – One way to confront this problem is to balance circadian rhythm.
Inflammation: A heart and cardiovascular risk characteristic not to be overlooked
Factors to be aware of:
- stress
- viruses
- hydrogenated/trans-fats
- Omega 6 and Omega 3 inbalances
- Refined sugar
Video: Why you should focus more on inflammation than cholesterol?
Inflammation is probably one of the best markers for determining if you have or are at risk of heart disease. Which suggests that, regardless of cholesterol levels, arterial plaques will build up as a healing response to the locality of the inflammation.
This would also indicate that if you don’t have extreme inflammation, then the cholesterol can then flow freely through the bloodstream without depositing onto the arterial walls.
In a 2017 study from Brigham and Women’s Hospital, the findings showed that reducing inflammation and NOT lowering cholesterol, revealed a decrease in cardiovascular risk.
The book “The Great Cholesterol Myth ” is a read contending (for example) that lowering your cholesterol won’t prevent a declining heart/cardiovascular condition. This book has some very glowing reviews and covers 100 recipes for reducing inflammation and other heart disease risks.
What women should know to better manage heart health
In the podcast below, credentialed physician, Dr. Mark Menolascino gives some very thorough insights into how women can better understand and confront their heart health.
Here is list of key talking points:
- 2 out of 3 women suffer from heart disease
- Why is the first sign of heart disease in half of women death
- Understanding epigenetics as it relates to heart disease
- Why half of heart attacks occur with normal cholesterol levels
- Treating the individual according to the individual’s needs
- Accounting for inflammation
And much more…. listen here
sources: 2,3,4,6,7,8,9,10,11,13,14,16,22
Observations And Analysis
My takeaways in probing through dozens of articles over several weeks in order to obtain a more in depth perspective on weighing out the pros and cons of cholesterol and heart health, has brought me to some interesting key points.
Cholesterol and lipoproteins
In established medicine and science it is commonplace to refer to LDL and HDL as component of cholesterol. They are commonly referred to as LDL cholesterol and HDL cholesterol.
I find this to be misleading due to the fact that lipoproteins are NOT cholesterol and cholesterol is NOT a lipoprotein.
These are two separate entities that should be segregated when determening heart attack, cardiovascular and stroke concerns. When you get a total cholesterol test, you are testing for a number of other elements in addition to cholesterol itself.
Examining inflammation as opposed to cholesterol
This is probably the most pertinent aspect of the research compiled for this article. Looking further into the elements that are responsible for triggering inflammation, in my estimation, appears to be the most practical and sound strategy for investigating the dangers of heart and cardiovascular health.
Awareness of the items mentioned earlier which can (amoung other things) be a causality for free radical damage (leading to inflammation) as well as dietary/lifestyle adjustments, I do believe, are quality steps in the right direction. Additionally, the aforementioned c reactive protein test ( i would submit) is wise choice to give you some scope of where you are with inflammation as it relates to the the health of your arteries and heart.
Thoughts on the researched dangers of High HDL
In the studies alluded to earlier, the results reveal, at first glance, that raising HDL levels with lowered LDL and triglyceride levels do nil to reduce heart disease, heart attack or stroke risk.
Ok. So, the studies were performed using a niacin derivative drug called Niaspan. As I reported earlier, this drug has been associated with numerous side effects. Not the least of which, toxicity and inflammation to the liver.
I would gather that it is reasonable to suspect that a drug, such as this, that would have adverse effects to the health of your liver, could have something to do with the lack of a positive outcome in the study.
Whereas, if the study was performed using a more safe method for raising HDL and lowering LDL and triglyerides, one wonders, maybe the results would be different.
Ascertaining the link between atherosclerosis and cholesterol
In an earlier subsection we went over various published studies premised on finding a link between atherosclerosis and cholesterol.
In all the data sifted through and presented, there are published findings that show a connection confirming at least a small difference in higher cholesterol in autopsies of subjects that revealed atherosclerosis and other findings that showed no connection.
If these studies are based on total cholesterol’s relationship therein and not isolating lipid and triglyceride levels, then these statistics could be inconclusive on both sides of the argument.
The bottom line in my summation is that the data seems to be somewhat anecdotal in regards to definitively identifying that high cholesterol alone and atherosclerotic plaque are correlated.
Update 02/23/21: More On Cholesterol
Note from the editor: As is mentioned below in the “final thoughts” section of this piece, there is a vast amount of data involving factual and conjectured information on this particular subject. With that said, there is so much more that could have been presented here (as I allude to in the below section).
So on that note, i was approached recently with some more data that cites many facts, figures, statistics and particulars on the topic that lend to many angles that I did not cover. I believe this information, in the link I provide below, has a lot of value in furthering your knowledge base beyond what is published here.
Speaking for myself, I learned a lot and am grateful to the author of this piece for reaching out for me to share. I would highly implore you the reader to take some time to review this article and learn more on this topic. Read here
Final thoughts
In researching an extensive amount of content to complete this article, I’ve come to a much better and broader comprehension of this particular topic.
Though it may seem like overkill to cite so many referenced sources (by far the most of any of my posts), I felt it was necessary to do so in order to provide a comprehensive scope in order to give a sense of direction as to what you (as an individual) might want to consider as a course of action in attending to heart health and arterial health.
Moreover, understanding where cholesterol plays into the picture therein, is a big central motivation.
With that said, though there is a lot of information that i sifted through there is also much information that wasn’t and (probably should have been) in this report, and (or) completely overlooked, which, I’m sure, has left at least a few loose ends that could have been covered.
This is where I would implore you, the reader, to offer your thoughts, facts and findings on this topic if you believe the information is conjecture, incorrect or was not covered or not covered thoroughly enough.
So please offer your comments below, so if necessary, I can edit and update the particular facets and fine tune the accuracy of the content in the interest of truth and clarity.
One last point
As I do in all my posts, I always recommend that you discuss the content I present with your doctor moving forward. Especially, if it is applicable to your best health interests.
I believe this is especially paramount, as compared to my other posts, based on the information presented.
The various methods of testing mentioned earlier here (in my mind) are wise in terms of arming your knowledge base, so you can ask your physician about the options and logistics of getting these particular tests done.
Speaking for myself, these are questions I will be prepared to ask during my next doctor visit.
Thank you for reading, and again, if you have any thoughts to offer please leave them below.
Onwards and upwards with your health!
Sourced references:






I found your article very informative. I am overweight and worry about my cholesterol quite often. I read all the way to the end because this information is important to me. I have been given a lot of conflicting advice and information over the years. It was nice to have it broke down for me. I feel able to make better decisions when it comes to what and how much cholesterol I consume. thanks again.
Thanks for taking the time to read and comment. It took a ton of research and vetting to complete this dissertation for presentation. I’m so glad you thoroughly read this and has assisted in giving you further scope on how to look at cholesterol and heart/cardiovascular health. Which is the premise for writing this post.
Blessings with gratitude, Brad
You did your homework. Thank you for the research and getting this important information out to the public. My cholesterol is high and when my arteries were tested (lovely) they were clear. The doctor I had at the time pushed me to take the statin drugs. I refused and my new doctor agrees with me about them.
I read the Great Cholesterol Myth too. Most of the physicians on the FDA panel deciding that statins were a good thing owned stock in the drug companies manufacturing the statins.
And I wonder about if the statin drugs are at least a contributing factor in the dramatic rise in Alzheimer’s and diabetes.
Wow Suzanne,
You said a mouth full!
It’s so good to see that the the extent of research in gathering and compiling this data doesn’t go unnoticed.
So, your cholesterol is high and your arteries are clear? Well there you go… that’s the conclusion that many of the published studies and other data have published as well.
The FDA and the drug companies are in collusion together. I have no doubt that there is “revolving door” contingent going where these FDA administrators go to work for these drug companies and vise versa. I call it medical fascism. It’s all the same animal.
I would say yes, statins being responsible for Alzheimer’s and diabetes is highly plausible (to put it mildly) and well documented. The Brain needs cholesterol to function efficiently. I’d say that makes for compelling evidence that when you artificially lower cholesterol it’s bound to eventually take a toll on the brain’s functionality among so many other factors.
I appreciate all the great point you made here.
Thank you with much gratitude, Brad
Thank you for this detailed look at cholesterol. When I was in cooking school we were taught that if the body does not get enough cholesterol through diet, it can make as much as it needs.
It seems unbelievable that the medical community would not know about this, and yet they push people to lower their cholesterol because heart disease could not possibly be caused by a low fat diet. It is shocking how unhealthy everyone has become due to this “advice”.
Thank you for being a voice of reason!
Thank you for your perspective Irma. I can see that you have an interesting angle on this as to information you learned in cooking school. I think this all has to do with the medical industrial complex’s bottom line which is not centered in restoring health by giving your body the ability to heal and sustain optimum health. Rather (and I think you know what i’m going to say) it’s profit. A healthy populace is detrimental to their cash cow.
I’m with you on your insights.
Blessings with gratitude and wishing you the best of health, Brad
What a nice post you wrote! I really enjoyed reading it and I could not be silent about your post so I decided to leave my comment here and say Thank You! For sharing this quality post with others.
Actually this is exactly the information that I was looking for about heart attack risk and when I landed to your website and read this post, it answered all my questions in details.
So I’m happy that you decided to write about this topic and share it with people. It’s very useful and can definitely be used as a great source for cholesterol effects on our body.
I will come back to your website again for sure and I’m looking forward to read your new posts.)
Thanks!
Thank you so much for your time and comment Ali. I’m glad you got some constructive perspective out of this piece. It took many hours of research to put this together. So, I am very grateful for your kind words.
Cheers and blessings,Brad
Very interesting points of view on the whole cholesterol dilemma. I’ve researched the subject extensively before and because of the vast amount of conflicting studies it was impossible to form a conclusive opinion. I’m from Finland and there are some epidemiological studies done for several decades on the men from eastern parts of our country. This is because in the past they all tended to die out of heart disease before hitting 50. One conclusion they came to in those studies is that they got the vast majority of their daily calories from lard, cream and other saturated animal fat sources. Most study subjects did extremely demanding manual labor like cutting timber, construction or farming and consumed anywhere between 5000 to 10 000 calories per day, mostly from fat. Reducing the dietary saturated fat their life expectancy improved significantly. I’ve read criticism on these studies that they didn’t take into account other lifestyle factors like smoking, alcohol consumption and overall physical, mental and emotional stress levels. I think this is a very complex issue with several different disease factors and cholesterol is just one of those factors. Genetics, diet and lifestyle seem to affect how well cholesterol levels correlate with heart disease risk. And cholesterol(s) definitely have an important biological function and reducing them blindly doesn’t seem wise. I’ll have to go through your post and sources with more detail when I have more time!
Thank you Jukka for reading and weighing in. These are the type comments i’m looking for in regards to adding more angles that i may have not covered thoroughly enough. Especially when someone like yourself who has spent a considerable amount of time studying the topic. Finding that smoking gun, red pill conclusion was difficult for me as well. This was a mentally exhausting and challenging post to complete and as I said in my observation, there is a lot of slants that i did not look into deeply enough. Which is why comments like yours are very valuable.
It is interesting what you mention the about the studies showing how high saturated fat intake is connected to heart disease deaths before 50. I came across some data that supports this although, maybe i didn’t look into it as thoroughly as I should have. I cited a study from Harvord in 2013 that showed saturated fat as less invasive to heart risk than total fat. My question is that how much of the dietary intake came from dairy fats. There is a lot of conjecture about how dairy fat is responsible for inflammation and other health issues. I touched on this briefly. The late Dr. Christopher points out that it is like a GLUE in your system that can gum up inside of you causing allergies inflammatory responses, leaky gut ect… He goes on to say that Elmer’s glue is extracted from dairy milk. I always wondered why they show a cow on their product. But that is contested topic as well. I believe there are many out there who are able to secrete lactose/milk solids fine and others who don’t.
So, all in all, one of my big takaways in researching this subject in regard to how you handle cholesterol management is, an individuals metabolism and genetics are unique from person to person. It’s not as simple as just raising or lowering your cholesterol for the wellbeing of your heart and circulation. As you said it’s very complicated.
At any rate… Thank you so much for adding your two cents and your findings on the subject,
Blessings to your good health, Brad
Many of the symptoms and signs of Aortic Stenosis may be incorrectly attributed to the normal ageing process. It is this common misconception that keeps patients from discussing these symptoms with their families and Doctors. It is important to ensure that anyone with these symptoms should be referred to their local Doctor for assessment. symptoms of Aortic Stenosis
Hi Aliston,
Thank you for commenting on my post and adding your perspective. This is a very complicated topic. I’m glad to learn more about Aortic Stenosis. The link you provided is valuable in further educating myself and my readers.
Thanks again and blessings, Brad